New research has shown the connection between stomach and intestinal issues with depression and anxiety and a sense of well-being.
THE INTESTINAL MUCOSA is covered by a mucus gel layer that plays important physiological roles including lubrication, protection against colonization by pathogenic bacteria and their toxins, protection against luminal proteases arising from bacterial and mucosal cells, and constitution of a diffusion barrier for small molecules
Colonic mucus cells are located in the vicinity of enteric nerves, enteroendocrine cells, and resident immune cells, which suggests a potential role of neurotransmitters, hormonal peptides of the large bowel, and inflammatory mediators.
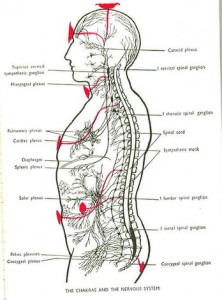
The Brain-Gut Connection
- Every known neurotransmitter present in the brain is present in the gut
- The gut is the most 'nervous' organ in the body or is that nervy? It's got a lot of innervation!
- The gut has independent mechanisms from the brain to regulate actions [enteric nervous system ENS]
New research has shone the connection between the stomach and intestinal issues with depression and anxiety as well as a sense of well-being.
95% of your serotonin is made in the intestines. Both anxiety and depression as well as sleep disorders can be related to low serotonin levels. Serotonin is just one of many neurotransmitters that are important in a person's overall sense of well-being.
Nerves have a language similar to speech. The alphabet of this language is the neurotransmitter. The location and amount of neurotransmitters secreted are the language spoken to the brain. Our nerves learn the language by repetitive stimulation.
Neurotransmitters
Neurotransmitters send signals throughout the nervous system. We used to think these chemicals, such as dopamine and serotonin, resided in the brain at the end of nerve cells. We now know that they can be found in many other organs--the heart, the gut, the immune system--and that they can diffuse out into the tissues and the blood. This is why so much of what happens to us shows up in many different parts of the body; why depression, associated with low serotonin levels in the brain, also causes decreased immune function and decreased bowel function, and why anti-depressants can have gastrointestinal side effects.
The Second Brain
- The GI tract 'is' a second brain which is somewhat independent of, but interaction with, the brain in the cranium
- Independent of guidance from the head, the gut can secrete, contract and respond to stimuli such as distention.
- Communication is a two-way street up and down from brain to gut
Unknown to most people, we actually have two physical brains. You're intimately familiar with the brain encased in your skull. But did you know you also have a second brain in your gut?
Actually, over one half of your nerve cells are located in your gut.
And you may be even more surprised to learn that your second "gut brain" contains neurons and neurotransmitters just like those found in your skull.
Plus here's something that may come as even more of a shock! Just like your primary brain, your "gut brain" is also able to learn, remember, and produce emotion-based feelings.
The expression "gut-level feeling" isn't just a "saying." We really do have feelings in our gut.
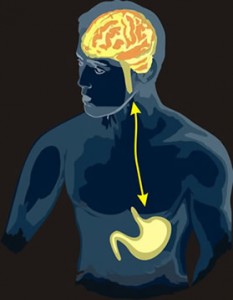
Our two brains communicate back and forth via a major nerve trunk extending down from the base of your brain all the way down into your abdomen. Because of this, your two brains directly influence each other.
When one brain becomes upset, the other joins right in.
That's why your stomach might get "fluttery" because of anxiety before an important meeting. Or why a late night spicy snack that's hard on your stomach might also give you some nasty nightmares.
In "The Second Brain," Dr. Michael Gershon, a professor at New York City's Columbia-Presbyterian Medical Center, refers to the entire gastrointestinal system as "the body's second nervous system."
"The brain is not the only place in the body that's full of neurotransmitters," Dr. Gershon explains. "One hundred million neurotransmitters line the length of the gut -- approximately the same number found in the brain."
Actually, the total of nerve cells in your gut is greater than the total nerves connecting the rest your body to your brain. This complex circuitry allows your "gut brain" to act totally independent of the brain in your skull.
It is no surprise that there is a direct relationship between emotional stress and physical distress. "Clinicians are finally acknowledging that a lot of dysfunction in GI disorders involves changes in the central nervous system," said Gary Mawe, a professor of anatomy and neurobiology at the University of Vermont.
The big question is which comes first, physiology or psychology?
The enteric (GUT) and central nervous systems use the same hardware, as it were, to run two very different programs. Serotonin, for instance, is crucial to feelings of well-being.
But 95 percent of the body's serotonin is housed in the gut, where it acts as a neurotransmitter and a signaling mechanism. The digestive process begins when a specialized cell, an enterochromaffin, squirts serotonin into the wall of the gut, which has at least seven types of serotonin receptors. The receptors, in turn, communicate with nerve cells to start digestive enzymes flowing or to start things moving through the intestines.
Either way, what is good for one brain is often good for the other, too. A team of researchers from Penn State University recently discovered a possible new direction in treating intestinal disorders, biofeedback for the brain in the gut.
To put this simply: problems in your digestive system can be a source of not only emotional issues but even disorders like autism. Even disorders that are considered IMMUNE system disorders like rheumatoid arthritis could be caused by digestive system disorders.
The good news is chiropractic adjustments, diet and nutritional therapy are the most effective treatment for the digestive system.
Things to consider.
Diet Tips
o Identify and avoid trigger foods.
o Practice conscious eating. Take time to savor food, chew thoroughly, and enjoy eating as a ritual.
o Don't lie down right after a meal.
o Maintain a healthy weight.
Stress
o Create calm. Turn off the television or computer during mealtimes.
o Learn and practice relaxation techniques.
Exercise
o Exercise tones the intestines.
o Get regular. Aim for 30 to 60 minutes.